Summary
Learning you have colorectal cancer (CRC) can be overwhelming — especially when words like “biomarkers” or “HER2” start coming your way. This FAQ highlights key takeaways from Fight CRC’s webinar, “Understanding HER2: What Patients Need to Know,” with answers from experts and advocates. Whether you’re newly diagnosed or exploring treatment options, this guide can help you understand HER2 and why it matters for your care.
Understanding HER2: What Patients Need to Know
Understanding HER2: What Patients Need to Know
Understanding HER2: What Patients Need to Know
Summary
Learning you have colorectal cancer (CRC) can be overwhelming — especially when words like “biomarkers” or “HER2” start coming your way. This FAQ highlights key takeaways from Fight CRC’s webinar, “Understanding HER2: What Patients Need to Know,” with answers from experts and advocates. Whether you’re newly diagnosed or exploring treatment options, this guide can help you understand HER2 and why it matters for your care.
Frequently Asked Questions from the Fight CRC Webinar
How planning ahead, tracking symptoms, and leaning on your care team can keep you stay strong through treatment.
Learning you have colorectal cancer (CRC) can be overwhelming — especially when words like “biomarkers” or “HER2” start coming your way. This FAQ highlights key takeaways from Fight CRC’s webinar, “Understanding HER2: What Patients Need to Know,” with answers from experts and advocates. Whether you’re newly diagnosed or exploring treatment options, this guide can help you understand HER2 and why it matters for your care.
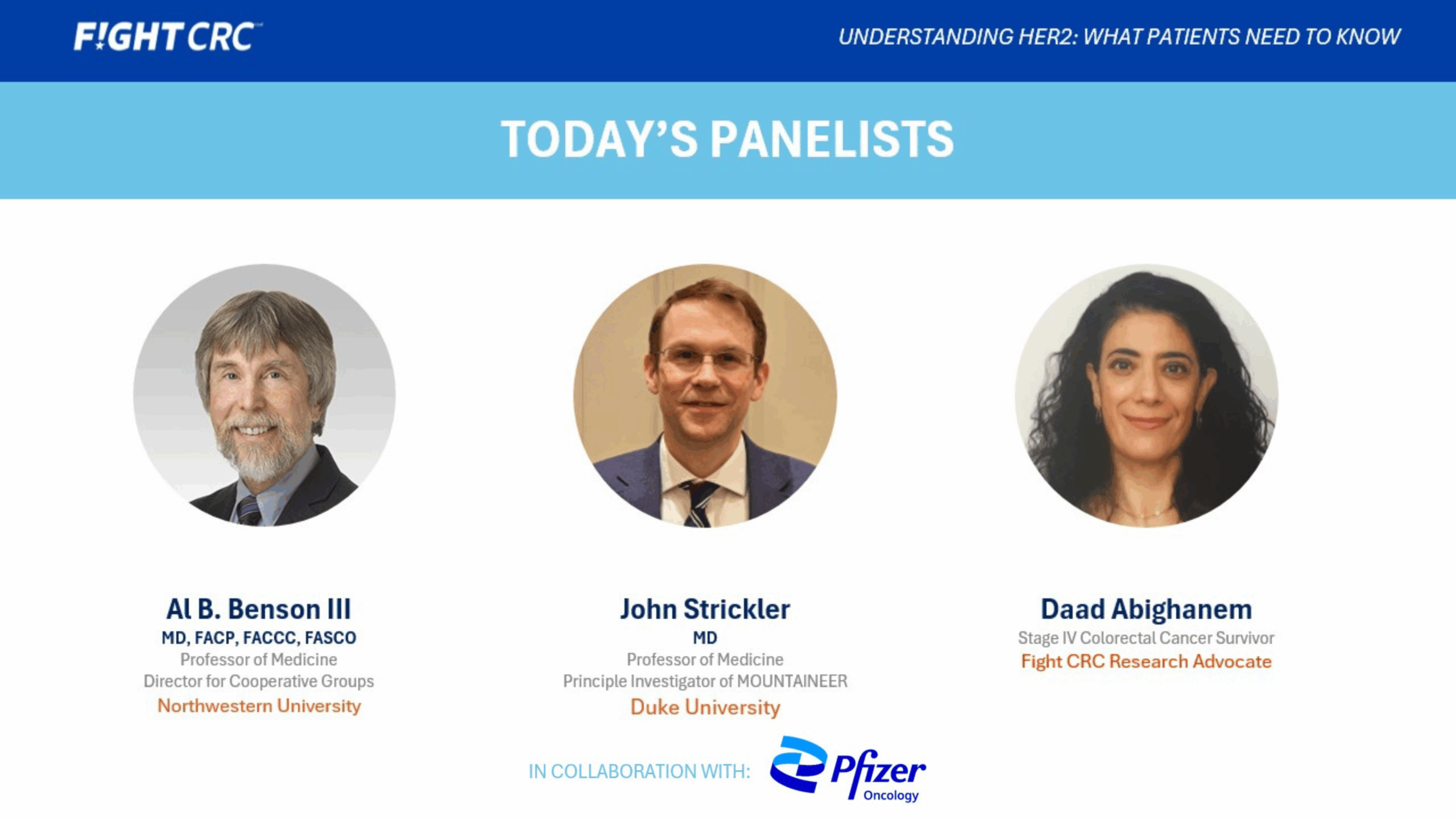
Featuring:
- Dr. John Strickler (Duke University)
- Dr. Al Benson (Northwestern University)
- Daad Abighanem, Fight CRC Research Advocate and Stage IV Survivor
Together, they shared insights on testing, treatment, advocacy, and how to take charge of your care if you or your loved one is affected by HER2-positive colorectal cancer.
What is HER2 and why does it matter?
HER2 (short for Human Epidermal Growth Factor Receptor 2) is a gene that helps cells grow and divide. In some colorectal cancers, the HER2 gene makes too many copies of itself — this is called HER2 amplification. When this happens, cancer cells get constant “grow” signals, making them multiply faster.
HER2 is important because it can affect how the cancer behaves and responds to certain treatments. Around 3–5% of people with metastatic colorectal cancer (mCRC) have HER2-positive disease. Knowing your HER2 status helps your care team choose treatments that are more likely to work for you.
Bottom line: Knowing your HER2 status can change your treatment plan and possibly your outcome.
How do I get tested for HER2?
HER2 testing is part of biomarker testing, which looks for changes in your tumor’s genes or proteins. Testing is now recommended for everyone with metastatic colorectal cancer, especially those with RAS and BRAF wild-type and microsatellite stable (MSS) tumors.
Common tests include
• IHC (Immunohistochemistry): Looks for too much HER2 protein on cancer cells.
• FISH or ISH (In Situ Hybridization): Checks if there are extra copies of the HER2 gene.
• NGS (Next Generation Sequencing): a broad genetic test that identifies HER2 and other biomarkers.
A tumor is considered HER2-positive if it’s scored as IHC 3+, or IHC 2+ with gene amplification on ISH testing.
Ask your doctor: “Have I had biomarker testing that includes HER2?”
If not, visit FightCRC.org and use our Provider Finder tool to locate specialists experienced in biomarker-driven care.
What treatments are available for HER2 positive colorectal cancer?
There are now FDA approved HER2-targeted treatments for colorectal cancer — an exciting step forward in precision medicine, giving patients more time and more options.
Common treatments include:
- Tucatinib + Trastuzumab (approved 2023 – based on the MOUNTAINEER trial): This combination has shown to shrink tumors and help patients live longer, with manageable side effects.
- Trastuzumab Deruxtecan (T-DXd): A next-generation antibody-drug conjugate that delivers chemotherapy directly to HER2-positive tumor cells.
Your eligibility will depend on your test results, treatment history, and overall health.
Ask your oncologist whether HER2 targeted therapy could be part of your treatment plan.
I feel overwhelmed by my biomarker results. What should I do?
You’re not alone—biomarker results can feel confusing and emotional at first. Take a breath and remember: these results are powerful tools to help your care team find the right treatment for you.
Our experts share this advice:
Dr. John Strickler: “It’s normal to feel overwhelmed. Ask your doctor questions and don’t stop until you understand the answers. Fight CRC’s Resource Library and patient community are great places to start.”
Dr. Al Benson: “Bring a family member or friend to appointments to take notes. Review your results together afterward, and always clarify what’s unclear.”
Daad A.: “It’s okay to feel afraid. Understanding your biomarkers gives you back control. It helps you make decisions with confidence and become an active partner in your care.”
How can caregivers and advocates support patients on HER2 targeted therapy?
HER2 positive colorectal cancer is relatively rare, and it can help to have extra support from your care circle.
Dr. Strickler: “Caregivers can attend visits, take notes, and ask questions. Partner with the medical team to ensure the patient gets the most up to date care.”
Dr. Benson: “Caregivers should know what side effects to watch for and how to manage them. Communication with the care team is essential.”
Daad A.: “Advocates and caregivers can connect patients with others who’ve walked this path. Shared experience can bring hope, reduce fear, and build community.”
How many HER2 targeted treatments can patients receive?
There isn’t a set limit. Your treatment plan depends on:
- What therapies you’ve already had
- How your cancer responds
- How your body tolerates the medicines
Doctors may start with Tucatinib + Trastuzumab, and if the cancer grows or changes, move on to Trastuzumab Deruxtecan (T-DXd) or a clinical trial. Your care team will personalize each step to what works best for you.
What are some barriers to testing or clinical trial participation?
Despite progress, many patients still face challenges, including:
- Limited awareness of biomarker testing or its importance
- Cost or insurance coverage issues
- Distance from major cancer centers – testing may not be available everywhere
- Fast-changing science – so not all providers are up to date
- Logistical barriers like travel or childcare
- Mistrust of research or fear of “experimental” care
- Language and cultural barriers
That’s why equal access to biomarker testing and clinical trials is so important. Fight CRC works to close these gaps through education, advocacy, and patient support.
How does advocacy make a difference?
Advocacy is the heart of progress.
By raising awareness, sharing stories, and pushing for equity, advocates help shape the future of colorectal cancer care and research.
Programs like Fight CRC’s Research Advocacy Training and Support (RATS) prepare survivors and caregivers to have a seat at the research table—influencing studies, clinical trials, and policies that change lives.
Daad A.: “Advocacy is self-care. When you speak up for yourself, you’re also helping the next generation of patients.”
Fight CRC Resources and Next Steps
Learn:
- Resource Library: Download guides on biomarkers, clinical trials, and treatment options
- Biomarker Testing Guide: Understand what testing involves and what results mean
- Biomarker Testing Guide: Understand what testing involves and what results mean
Connect
- Community of Champions App: Connect with patients and caregivers who “get it”
- Ambassador Program: Share your story and raise awareness
Advocate
- RATS Program (Research Advocacy Training and Support): Learn how to become a research advocate
- Call-on Congress: Join us this March in Washington, DC to push for policies that improve access and advocate for colorectal cancer research funding
Stay Informed
- Subscribe to the Clinical Trials Newsletter to receive the latest updates on HER2 and other emerging treatments.
Thank You to Our Sponsor
This webinar and FAQ were made possible through the generous support of Pfizer. Their partnership helps Fight CRC continue providing trusted education and empowering patients to make informed decisions about their care.
Summary
Learning you have colorectal cancer (CRC) can be overwhelming — especially when words like “biomarkers” or “HER2” start coming your way. This FAQ highlights key takeaways from Fight CRC’s webinar, “Understanding HER2: What Patients Need to Know,” with answers from experts and advocates. Whether you’re newly diagnosed or exploring treatment options, this guide can help you understand HER2 and why it matters for your care.
Frequently Asked Questions from the Fight CRC Webinar
How planning ahead, tracking symptoms, and leaning on your care team can keep you stay strong through treatment.
Learning you have colorectal cancer (CRC) can be overwhelming — especially when words like “biomarkers” or “HER2” start coming your way. This FAQ highlights key takeaways from Fight CRC’s webinar, “Understanding HER2: What Patients Need to Know,” with answers from experts and advocates. Whether you’re newly diagnosed or exploring treatment options, this guide can help you understand HER2 and why it matters for your care.
Featuring:
- Dr. John Strickler (Duke University)
- Dr. Al Benson (Northwestern University)
- Daad Abighanem, Fight CRC Research Advocate and Stage IV Survivor
Together, they shared insights on testing, treatment, advocacy, and how to take charge of your care if you or your loved one is affected by HER2-positive colorectal cancer.
What is HER2 and why does it matter?
HER2 (short for Human Epidermal Growth Factor Receptor 2) is a gene that helps cells grow and divide. In some colorectal cancers, the HER2 gene makes too many copies of itself — this is called HER2 amplification. When this happens, cancer cells get constant “grow” signals, making them multiply faster.
HER2 is important because it can affect how the cancer behaves and responds to certain treatments. Around 3–5% of people with metastatic colorectal cancer (mCRC) have HER2-positive disease. Knowing your HER2 status helps your care team choose treatments that are more likely to work for you.
Bottom line: Knowing your HER2 status can change your treatment plan and possibly your outcome.
How do I get tested for HER2?
HER2 testing is part of biomarker testing, which looks for changes in your tumor’s genes or proteins. Testing is now recommended for everyone with metastatic colorectal cancer, especially those with RAS and BRAF wild-type and microsatellite stable (MSS) tumors.
Common tests include
• IHC (Immunohistochemistry): Looks for too much HER2 protein on cancer cells.
• FISH or ISH (In Situ Hybridization): Checks if there are extra copies of the HER2 gene.
• NGS (Next Generation Sequencing): a broad genetic test that identifies HER2 and other biomarkers.
A tumor is considered HER2-positive if it’s scored as IHC 3+, or IHC 2+ with gene amplification on ISH testing.
Ask your doctor: “Have I had biomarker testing that includes HER2?”
If not, visit FightCRC.org and use our Provider Finder tool to locate specialists experienced in biomarker-driven care.
What treatments are available for HER2 positive colorectal cancer?
There are now FDA approved HER2-targeted treatments for colorectal cancer — an exciting step forward in precision medicine, giving patients more time and more options.
Common treatments include:
- Tucatinib + Trastuzumab (approved 2023 – based on the MOUNTAINEER trial): This combination has shown to shrink tumors and help patients live longer, with manageable side effects.
- Trastuzumab Deruxtecan (T-DXd): A next-generation antibody-drug conjugate that delivers chemotherapy directly to HER2-positive tumor cells.
Your eligibility will depend on your test results, treatment history, and overall health.
Ask your oncologist whether HER2 targeted therapy could be part of your treatment plan.
I feel overwhelmed by my biomarker results. What should I do?
You’re not alone—biomarker results can feel confusing and emotional at first. Take a breath and remember: these results are powerful tools to help your care team find the right treatment for you.
Our experts share this advice:
Dr. John Strickler: “It’s normal to feel overwhelmed. Ask your doctor questions and don’t stop until you understand the answers. Fight CRC’s Resource Library and patient community are great places to start.”
Dr. Al Benson: “Bring a family member or friend to appointments to take notes. Review your results together afterward, and always clarify what’s unclear.”
Daad A.: “It’s okay to feel afraid. Understanding your biomarkers gives you back control. It helps you make decisions with confidence and become an active partner in your care.”
How can caregivers and advocates support patients on HER2 targeted therapy?
HER2 positive colorectal cancer is relatively rare, and it can help to have extra support from your care circle.
Dr. Strickler: “Caregivers can attend visits, take notes, and ask questions. Partner with the medical team to ensure the patient gets the most up to date care.”
Dr. Benson: “Caregivers should know what side effects to watch for and how to manage them. Communication with the care team is essential.”
Daad A.: “Advocates and caregivers can connect patients with others who’ve walked this path. Shared experience can bring hope, reduce fear, and build community.”
How many HER2 targeted treatments can patients receive?
There isn’t a set limit. Your treatment plan depends on:
- What therapies you’ve already had
- How your cancer responds
- How your body tolerates the medicines
Doctors may start with Tucatinib + Trastuzumab, and if the cancer grows or changes, move on to Trastuzumab Deruxtecan (T-DXd) or a clinical trial. Your care team will personalize each step to what works best for you.
What are some barriers to testing or clinical trial participation?
Despite progress, many patients still face challenges, including:
- Limited awareness of biomarker testing or its importance
- Cost or insurance coverage issues
- Distance from major cancer centers – testing may not be available everywhere
- Fast-changing science – so not all providers are up to date
- Logistical barriers like travel or childcare
- Mistrust of research or fear of “experimental” care
- Language and cultural barriers
That’s why equal access to biomarker testing and clinical trials is so important. Fight CRC works to close these gaps through education, advocacy, and patient support.
How does advocacy make a difference?
Advocacy is the heart of progress.
By raising awareness, sharing stories, and pushing for equity, advocates help shape the future of colorectal cancer care and research.
Programs like Fight CRC’s Research Advocacy Training and Support (RATS) prepare survivors and caregivers to have a seat at the research table—influencing studies, clinical trials, and policies that change lives.
Daad A.: “Advocacy is self-care. When you speak up for yourself, you’re also helping the next generation of patients.”
Fight CRC Resources and Next Steps
Learn:
- Resource Library: Download guides on biomarkers, clinical trials, and treatment options
- Biomarker Testing Guide: Understand what testing involves and what results mean
- Biomarker Testing Guide: Understand what testing involves and what results mean
Connect
- Community of Champions App: Connect with patients and caregivers who “get it”
- Ambassador Program: Share your story and raise awareness
Advocate
- RATS Program (Research Advocacy Training and Support): Learn how to become a research advocate
- Call-on Congress: Join us this March in Washington, DC to push for policies that improve access and advocate for colorectal cancer research funding
Stay Informed
- Subscribe to the Clinical Trials Newsletter to receive the latest updates on HER2 and other emerging treatments.
Thank You to Our Sponsor
This webinar and FAQ were made possible through the generous support of Pfizer. Their partnership helps Fight CRC continue providing trusted education and empowering patients to make informed decisions about their care.
Summary
Learning you have colorectal cancer (CRC) can be overwhelming — especially when words like “biomarkers” or “HER2” start coming your way. This FAQ highlights key takeaways from Fight CRC’s webinar, “Understanding HER2: What Patients Need to Know,” with answers from experts and advocates. Whether you’re newly diagnosed or exploring treatment options, this guide can help you understand HER2 and why it matters for your care.
Frequently Asked Questions from the Fight CRC Webinar
How planning ahead, tracking symptoms, and leaning on your care team can keep you stay strong through treatment.
Learning you have colorectal cancer (CRC) can be overwhelming — especially when words like “biomarkers” or “HER2” start coming your way. This FAQ highlights key takeaways from Fight CRC’s webinar, “Understanding HER2: What Patients Need to Know,” with answers from experts and advocates. Whether you’re newly diagnosed or exploring treatment options, this guide can help you understand HER2 and why it matters for your care.
Featuring:
- Dr. John Strickler (Duke University)
- Dr. Al Benson (Northwestern University)
- Daad Abighanem, Fight CRC Research Advocate and Stage IV Survivor
Together, they shared insights on testing, treatment, advocacy, and how to take charge of your care if you or your loved one is affected by HER2-positive colorectal cancer.
What is HER2 and why does it matter?
HER2 (short for Human Epidermal Growth Factor Receptor 2) is a gene that helps cells grow and divide. In some colorectal cancers, the HER2 gene makes too many copies of itself — this is called HER2 amplification. When this happens, cancer cells get constant “grow” signals, making them multiply faster.
HER2 is important because it can affect how the cancer behaves and responds to certain treatments. Around 3–5% of people with metastatic colorectal cancer (mCRC) have HER2-positive disease. Knowing your HER2 status helps your care team choose treatments that are more likely to work for you.
Bottom line: Knowing your HER2 status can change your treatment plan and possibly your outcome.
How do I get tested for HER2?
HER2 testing is part of biomarker testing, which looks for changes in your tumor’s genes or proteins. Testing is now recommended for everyone with metastatic colorectal cancer, especially those with RAS and BRAF wild-type and microsatellite stable (MSS) tumors.
Common tests include
• IHC (Immunohistochemistry): Looks for too much HER2 protein on cancer cells.
• FISH or ISH (In Situ Hybridization): Checks if there are extra copies of the HER2 gene.
• NGS (Next Generation Sequencing): a broad genetic test that identifies HER2 and other biomarkers.
A tumor is considered HER2-positive if it’s scored as IHC 3+, or IHC 2+ with gene amplification on ISH testing.
Ask your doctor: “Have I had biomarker testing that includes HER2?”
If not, visit FightCRC.org and use our Provider Finder tool to locate specialists experienced in biomarker-driven care.
What treatments are available for HER2 positive colorectal cancer?
There are now FDA approved HER2-targeted treatments for colorectal cancer — an exciting step forward in precision medicine, giving patients more time and more options.
Common treatments include:
- Tucatinib + Trastuzumab (approved 2023 – based on the MOUNTAINEER trial): This combination has shown to shrink tumors and help patients live longer, with manageable side effects.
- Trastuzumab Deruxtecan (T-DXd): A next-generation antibody-drug conjugate that delivers chemotherapy directly to HER2-positive tumor cells.
Your eligibility will depend on your test results, treatment history, and overall health.
Ask your oncologist whether HER2 targeted therapy could be part of your treatment plan.
I feel overwhelmed by my biomarker results. What should I do?
You’re not alone—biomarker results can feel confusing and emotional at first. Take a breath and remember: these results are powerful tools to help your care team find the right treatment for you.
Our experts share this advice:
Dr. John Strickler: “It’s normal to feel overwhelmed. Ask your doctor questions and don’t stop until you understand the answers. Fight CRC’s Resource Library and patient community are great places to start.”
Dr. Al Benson: “Bring a family member or friend to appointments to take notes. Review your results together afterward, and always clarify what’s unclear.”
Daad A.: “It’s okay to feel afraid. Understanding your biomarkers gives you back control. It helps you make decisions with confidence and become an active partner in your care.”
How can caregivers and advocates support patients on HER2 targeted therapy?
HER2 positive colorectal cancer is relatively rare, and it can help to have extra support from your care circle.
Dr. Strickler: “Caregivers can attend visits, take notes, and ask questions. Partner with the medical team to ensure the patient gets the most up to date care.”
Dr. Benson: “Caregivers should know what side effects to watch for and how to manage them. Communication with the care team is essential.”
Daad A.: “Advocates and caregivers can connect patients with others who’ve walked this path. Shared experience can bring hope, reduce fear, and build community.”
How many HER2 targeted treatments can patients receive?
There isn’t a set limit. Your treatment plan depends on:
- What therapies you’ve already had
- How your cancer responds
- How your body tolerates the medicines
Doctors may start with Tucatinib + Trastuzumab, and if the cancer grows or changes, move on to Trastuzumab Deruxtecan (T-DXd) or a clinical trial. Your care team will personalize each step to what works best for you.
What are some barriers to testing or clinical trial participation?
Despite progress, many patients still face challenges, including:
- Limited awareness of biomarker testing or its importance
- Cost or insurance coverage issues
- Distance from major cancer centers – testing may not be available everywhere
- Fast-changing science – so not all providers are up to date
- Logistical barriers like travel or childcare
- Mistrust of research or fear of “experimental” care
- Language and cultural barriers
That’s why equal access to biomarker testing and clinical trials is so important. Fight CRC works to close these gaps through education, advocacy, and patient support.
How does advocacy make a difference?
Advocacy is the heart of progress.
By raising awareness, sharing stories, and pushing for equity, advocates help shape the future of colorectal cancer care and research.
Programs like Fight CRC’s Research Advocacy Training and Support (RATS) prepare survivors and caregivers to have a seat at the research table—influencing studies, clinical trials, and policies that change lives.
Daad A.: “Advocacy is self-care. When you speak up for yourself, you’re also helping the next generation of patients.”
Fight CRC Resources and Next Steps
Learn:
- Resource Library: Download guides on biomarkers, clinical trials, and treatment options
- Biomarker Testing Guide: Understand what testing involves and what results mean
- Biomarker Testing Guide: Understand what testing involves and what results mean
Connect
- Community of Champions App: Connect with patients and caregivers who “get it”
- Ambassador Program: Share your story and raise awareness
Advocate
- RATS Program (Research Advocacy Training and Support): Learn how to become a research advocate
- Call-on Congress: Join us this March in Washington, DC to push for policies that improve access and advocate for colorectal cancer research funding
Stay Informed
- Subscribe to the Clinical Trials Newsletter to receive the latest updates on HER2 and other emerging treatments.
Thank You to Our Sponsor
This webinar and FAQ were made possible through the generous support of Pfizer. Their partnership helps Fight CRC continue providing trusted education and empowering patients to make informed decisions about their care.