In 2011 at age 24, Ashley Flynn was diagnosed with stage III rectal cancer. For three years prior to her diagnosis, she had rectal bleeding and consulted multiple providers to determine the cause and solution.
Each of these providers suggested constipation, fissures, or hemorrhoids. Ashley tried creams and recommended remedies, none of which provided relief or resolved the bleeding.
After moving to a new city and establishing care with a new physician, Ashley’s doctor suggested she try MiraLAX® for two weeks. When the bleeding continued, Ashley’s doctor recommended a colonoscopy, where doctors discovered a large tumor in her rectum.
Her health care team recommended fertility preservation immediately, which Ashley underwent before beginning treatment. Today, she is in remission.
Ashley shares her fertility preservation experience to help other young, diagnosed patients have hope for parenthood after a colorectal cancer diagnosis.
Q: Did you or your medical team introduce the idea of fertility preservation?
A: My medical team brought up the topic of fertility preservation to me. At the time, it was another layer of confusion when all I wanted to do was survive my rectal cancer diagnosis.
When I was diagnosed, I was dating the man who became my husband. At the time, we didn’t have discussions about fertility preservation or family building.
It didn’t even cross my mind to preserve my fertility because I was in the survival mode of, “Let’s get treatment started tomorrow.” I didn’t want to wait.
I didn’t think of future children at the time, but I’m glad my medical team talked about my future and helped me plan for it.
Q: What guidance did you receive about fertility preservation?
A: I was told I could meet the fertility team quickly following my diagnosis. Because my family didn’t live close by, a friend went with me to my fertility preservation consulting appointment. I thought it would be good to have someone go with me to keep me company.
I wasn’t expecting the appointment to be complex, but it was. Even with my experience as a nurse and extensive medical knowledge, it was unexpectedly challenging. I felt like my world was turned upside down.
The specialist there made the waters even more muddy because I was this 24-year-old, newly diagnosed cancer patient, and they gave me what felt like too many options. I didn’t know what was best for me, and I wanted them to tell me what was best for me.
I was given some options:
- Freezing my eggs
- Removing an entire ovary, which at the time was experimental, yet I felt pushed hard to go in this direction
- I left that meeting confused and tearful. I didn’t know what to do. I also didn’t want to delay treatment.
I returned to my radiation oncologist. He told me chemotherapy wouldn’t be devastating to my ovaries, but radiation would be. He suggested ovarian transposition: a surgery that would lift my ovaries from my pelvis, closer to my abdomen and kidneys, out of the field of radiation.
That sounded like the best option, so he referred me to a gynecologist/oncologist who performed that surgery.
Under normal circumstances, I would have had a surgery consult where I met the surgeon, had the surgery explained, and then had the opportunity to ask questions. We didn’t have time for any of that.
In the span of 20 days, I was diagnosed, had ovarian transposition surgery, had a port placement, and began chemo.
Q: What led you to IVF to start your family?
A: First, I want to caution people: Never go to appointments by yourself. It’s always good to have someone else to listen and ask questions.
My IVF story is interesting.
While I was in treatment, I had always thought I would be able to have kids naturally because the ovarian transposition would be reversed after I completed treatment.
That was not the case.
 I learned in 2014 that once my ovarian transposition surgery was done, that was it. It couldn’t be reversed. Because of the surgery, we would need to have IVF to have children.
I learned in 2014 that once my ovarian transposition surgery was done, that was it. It couldn’t be reversed. Because of the surgery, we would need to have IVF to have children.
My treatment ended in August 2012. My husband and I got married in June 2015, and we began discussions with our doctor about six months later, since we knew we needed IVF to start our family.
The first time I took the medications to stimulate my ovaries, whenever an ultrasound was completed to monitor those ovaries for follicle growth, they could only find my right ovary. The right ovary wasn’t having the best response to the to the medications. There weren’t a lot of follicles available.
They attempted the egg retrieval anyway. At this point, the doctors thought they could still obtain my eggs vaginally.
The doctor went in to retrieve my eggs, and she said it felt like she was taking the needle and poking it through a wall.
My ovary was that hard.
After that procedure, I had the worst abdominal pain that I’ve ever felt in my life, and I ended up going to the emergency room.
My doctor brought me back in the next day for an ultrasound, and I remember when they were doing the ultrasound, my husband asked, “What was that?”
The radiology tech responded, “That’s her kidney.”
My husband responded, “No, that looks like an ovary.” The tech left the room to get the doctor.
Because we were going through this process and I was getting a lot of ultrasounds, my husband and I knew what an ovary with lots of follicles looks like. The doctor came in and said, “Yes. That is your ovary in your back.”
We had to go through the entire IVF process again because those eggs that they obtained from the rock-hard ovary did not grow. The doctors think that the right ovary had become detached from the oblique muscle and fell into the radiation field and was irradiated.
For the second egg retrieval, the doctor went in through my left side and took eggs from my left ovary. We ended up with one viable embryo. It only takes one embryo to make a baby.
Q. What has your IVF journey looked like?
A: My journey felt and looked like this:
- Doctors took my one embryo and placed it in the uterus.
- The embryo has to “stick” to become pregnant. This happened for me.
- The next phase is being sure hormone levels keep rising. Doctors continually monitored my hormones.
- Meanwhile, there’s an ultrasound to make sure there’s a heartbeat.
- There was always a “next phase.” There was always another step.
Fortunately, IVF was successful for us. My little boy, Sam, is 7, and he was born in January 2017.
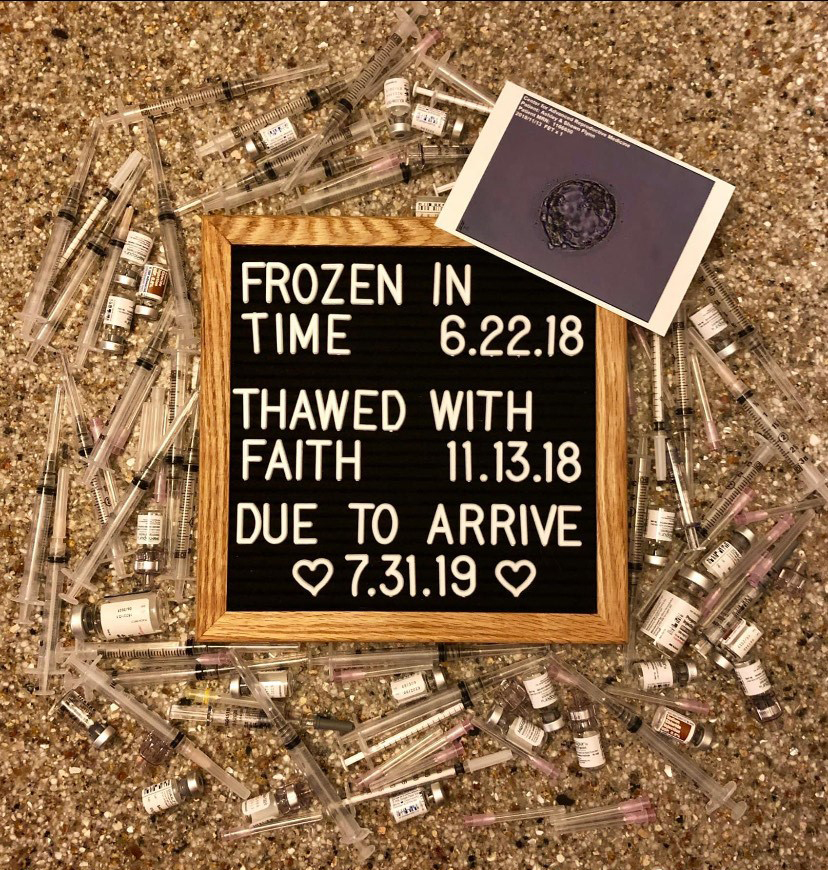
We knew we wanted more kids, but we had no more embryos, so we had to do the entire egg retrieval process again a few years later. From that egg retrieval, we got two embryos. The first embryo is my little boy Luke who is 4 now. He was born in July 2019.
We had one embryo left. In September 2021, we put that embryo in, and I miscarried.
Q: Did you ever feel frustrated or hopeless during your IVF journeys?
A: Yes. 100%.
I think when you’re going through your IVF journey, people think, “Oh, that girl has 10 eggs. That’s 10 kids that she could have.”
IVF is considered “successful” when you get pregnant with the embryo.
But that wasn’t my measure of success because that was not the end of my journey. I always said that I would never be happy until I had a baby in my arms.
Q: In hindsight, is there anything that you wish you could have done differently?
A: Yes. If I could do it over again, I would have frozen my eggs and then had the ovarian transposition surgery because I had some issues down the road.
I wish I had frozen my eggs, because in hindsight, my ovaries were affected by chemotherapy and radiation. Since my ovary had fallen into the radiation field, it was no longer functioning. This left me with one ovary. Women are born with all the eggs they will ever have in their lifetime. Although I still had one functioning ovary, in my opinion, it would have been beneficial to have eggs that had not received chemotherapy. This could have been done if I had frozen my eggs prior to receiving chemotherapy.
We struggled getting quality embryos. It took three egg retrievals to get three genetically normal embryos, two of which were successful. In an ideal world, a person would have one egg retrieval, get multiple eggs, and be able to use those to create multiple embryos. This is why I believe it would have been helpful to have an egg retrieval prior to receiving chemotherapy.
Q: Did your medical team discuss long-term effects of treatment with you?
A: While my radiation oncologist said radiation would be devastating to my ovaries, I was told absolutely nothing about long-term effects of treatment, as far as I remember. If they were discussed, I have no recollection because of being in the “newly diagnosed cancer patient fog.”
I was not advised that radiation would impact my ability to carry, but my colorectal surgeon was adamant that I did not deliver vaginally. Therefore, we planned for me to have a cesarean section (C-section). Doctors thought that the increased pressure from childbirth could rupture my previous surgical site in my rectum leading to life-long incontinence. I also believe there is a connection between radiation treatment and my sons coming before the planned C-section date.
Otherwise, I don’t have a lot of long-term side effects. My biggest issue is pelvic floor dysfunction from surgery. Of course, I do have some anxiety surrounding secondary cancer or relapse.
I recently reached out to a radiation oncologist friend and explained that I was never given my radiation doses or told what my long-term effects could be.
She went through details of my radiation with me. She explained that my uterus and bladder were directly in the radiation field, and they were the organs most affected.
Q: Did insurance cover IVF?
A: I work in a hospital, and I am fortunate that my insurance covered up to $10,000 total over a lifetime. Most employers do not have fertility coverage.
When we’re talking about IVF treatments, the money goes pretty quickly.
Finding a silver lining in the situation, Livestrong paid for medications, such as the injectables needed stimulate the ovaries. Medications to stimulate ovaries consisted of multiple injections, estrogen patches, estrogen tablets, and progesterone tablets. These medications were continuously monitored, measured, and adjusted depending on my lab results and follicle size/quantity. Livestrong has certain medications they will pay for, and our reproductive endocrinologist had other ones they preferred to use. Though Livestrong didn’t pay for all my medications, they paid for some.
I kept a running total of how much IVF cost us, which was about $17,000 to $20,000 out of pocket per kid.
As far as insurance and delivering babies: My medical team recommended planned C-sections. My health insurance would not approve a C-section until I reached 38 weeks, but neither of my pregnancies made it to my scheduled dates. Both were emergency C-sections.
I had Sam at 37 weeks. I went into labor with Luke at 35 weeks and six days. Since I delivered Luke after midnight, technically I delivered at 36 weeks (about 8 and a half months).
Q: What advice would you give to other colorectal cancer survivors who are considering IVF and carrying their own children after treatment?
A: Think about fertility preservation and your future.
Looking back, my health and saving my life was a priority. But it’s important to think about and hope for life after cancer.
I think of fertility preservation procedures as insurance plans: They are there if you need them, and hopefully, you’ll never need them. But it is always good to have a backup plan.Q: What are your hopes and dreams for the future?
A: I hope we find out why so many young adults and adolescents are being diagnosed with colorectal cancer so young
 My dream is every single cancer patient, no matter the diagnosis or age, should have a fertility preservation consult.
My dream is every single cancer patient, no matter the diagnosis or age, should have a fertility preservation consult.
Currently I’m on the fertility preservation team at the children’s hospital in my city, and there are fertility preservation options for males and females as young as 6 months old.
My hope is to raise happy, healthy little boys, who unfortunately must have their first colonoscopy at age 14, 10 years before I was diagnosed.
While I haven’t broken that news to them yet, I believe that knowledge is power, I’m going to do all I can to make sure that they don’t have to go through what I did.
Q: Are there resources available for family-building post-cancer?
A: There are a few programs and resources available to help. Some programs (such as the Expect Miracles Foundation SAMFund Family Building Grant) accept applications only within a brief window.

